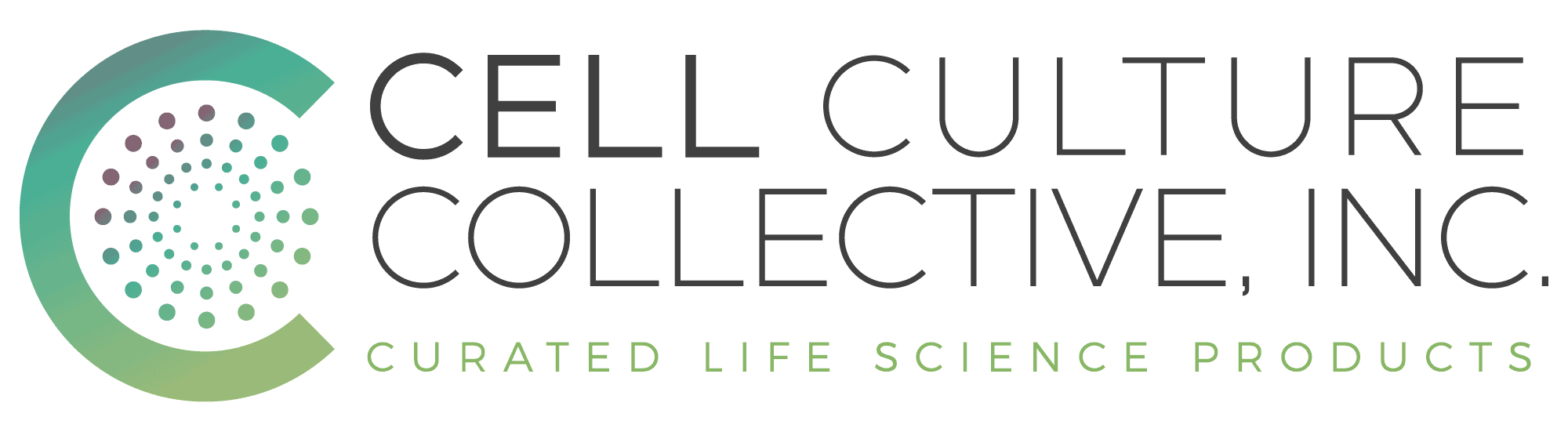
In laboratories around the world, cell cultures are integral to exploring the depths of biology, testing new treatments, and advancing medical research. However, despite the controlled environments, contamination remains one of the biggest hurdles researchers face, with circular contamination often being the most persistent and disruptive.
Circular contamination in cell culture refers to the unintended introduction of microorganisms, chemicals, or foreign cells that can jeopardize the entire experiment. It’s subtle at first, a slight change in medium color or an unexpected drop in cell growth, but left unchecked, it can compromise data reliability, waste time and resources, and derail progress.
Fortunately, contamination doesn’t have to be an inevitability. By identifying its causes and understanding effective prevention and mitigation strategies, researchers can maintain pristine cultures and achieve consistent, trustworthy results. In this guide, we’ll learn the root causes of circular contamination, how to spot it early, and actionable solutions to keep your cell cultures thriving.
Credit: AndreasReh / E+ / Getty
What is Circular Contamination in Cell Culture?
Circular contamination in cell culture refers to the introduction of unwanted elements such as microorganisms, chemicals, or even foreign cells into the culture system. This type of contamination disrupts the controlled environment needed for cell growth, often leading to compromised results and wasted resources.
Contamination can manifest in various ways. It might appear as a cloudy or discolored medium, abnormal cell growth, or a sudden decline in cell viability. These visible signs are usually just the tip of the iceberg. Contaminants can remain undetected for long periods, subtly affecting your experiment before their presence becomes obvious.
Types of Circular Contaminants
-
Microbial Contaminants
-
-
- These include bacteria, fungi, and mycoplasma. They are often introduced through contaminated reagents, poor aseptic techniques, or airborne exposure.
-
-
Chemical Contaminants
-
-
- Residues from disinfectants, impurities in reagents, or plasticware leachates can interfere with cell function, altering experimental outcomes.
-
-
Cross-Contamination
-
- Accidental mixing of cells from another culture can lead to overgrowth and a loss of experimental integrity. Shared equipment and improper handling are common culprits.
Credit: Lab Tips and Tricks
The Impact of Contamination
Even a tiny contamination can have widespread effects. Microbial contaminants can compete with cells for nutrients, release toxins, or change the culture’s pH, making it impossible to obtain reliable results. Similarly, cross-contamination can mask true findings by introducing variables you didn’t account for.
Common Causes of Circular Contamination in Cell Culture
Circular contamination doesn’t just happen, it’s the result of specific oversights or mishandlings in the lab. Understanding these causes is the first step to prevention.
🦠 1. Microbial Contaminants
Contaminants like bacteria, fungi, and mycoplasma are the most common culprits. They can sneak into your culture through:
- Contaminated reagents or media.
- Poor aseptic techniques, such as improper handling of pipettes.
- Airborne particles in an unfiltered environment.
Impact: Microbial contaminants compete with your cells for nutrients, produce toxic byproducts, and often lead to medium discoloration or cloudiness.
🔗 2. Cross-Contamination
When cells from another culture accidentally mix with your own, the results can be disastrous. This typically occurs due to:
- Shared equipment (e.g., incubators, biosafety cabinets).
- Mishandling or improper labeling of samples.
Impact: Cross-contamination often results in overgrowth, masking the true behavior of your target cells and skewing experimental results.
⚗️ 3. Chemical Contaminants
Chemical contamination might not be immediately obvious but can wreak havoc on your culture over time. Common sources include:
- Residual disinfectants on labware.
- Impurities in reagents or culture media.
- Leachates from plastic containers or tubing.
Impact: These contaminants alter cell behavior, metabolism, and even viability, making experimental outcomes unreliable.
Identifying Key Sources of Contamination
The root of most contamination issues lies in inconsistent practices, unmonitored lab environments, or overlooked details during culture preparation. By identifying these vulnerabilities, you can strengthen your protocols and protect your work.
Signs of Contamination to Watch For
Contamination in cell culture can be subtle at first, often manifesting as small, easily overlooked changes. However, its effects can quickly cascade, jeopardizing experiments and data integrity. Recognizing these signs early is essential for effective intervention.
1. Visual Indicators
- Cloudy or Turbid Medium: This is often the first visible sign of microbial contamination, such as bacteria or fungi. It may also indicate mycoplasma growth, which is harder to detect without magnification.
- Color Changes in the Medium: Many culture media contain pH-sensitive dyes that shift in color when pH levels are altered by contamination. For example, a medium turning orange or yellow could indicate acidification caused by bacterial growth.
- Unusual Precipitates or Particles: Floating debris or a film on the medium surface may signal fungal contamination or chemical reactions between media components.
2. Abnormal Cell Growth and Behavior
- Slower Growth Rates: Contaminants often compete with cells for nutrients, causing noticeable delays in cell proliferation.
- Morphological Changes: Cells may appear rounded, shrunken, or fragmented. For adherent cultures, contamination can cause cells to detach from the surface prematurely.
- Unexpected Cell Clumping: Cross-contamination or fungal infiltration may result in uneven cell distribution and clustering.
3. Changes in Culture Dynamics
- Altered Metabolism: Contaminated cultures may display unusual metabolic activity, such as higher lactate production or reduced glucose consumption.
- pH Imbalances: A sharp pH drop (indicated by media color changes) often accompanies microbial contamination, while slower pH drifts can result from chemical contaminants.
4. Confirmation Through Testing
When visual or behavioral signs aren’t conclusive, diagnostic testing can help confirm contamination:
- Microscopy: Phase-contrast or fluorescence microscopy can reveal bacteria, fungi, or mycoplasma.
- Molecular Techniques: PCR (Polymerase Chain Reaction) is widely used for detecting mycoplasma and other microorganisms.
- Culture-Based Methods: Sterility tests using nutrient-rich media can confirm bacterial or fungal growth over time.
- ELISA or ATP Detection Kits: Sensitive methods for detecting microbial contaminants or deviations in cell health.
The Importance of Vigilance
Failing to identify contamination early can lead to:
- Compromised Data Quality: Contaminants introduce uncontrolled variables that skew results, often rendering experiments invalid.
- Resource Wastage: Valuable time, reagents, and funding are lost when cultures must be discarded.
- Extended Recovery Time: Contamination in shared lab spaces can spread, affecting multiple projects and researchers.
By keeping a close eye on your cultures and employing regular testing, you can detect contamination early and take timely corrective actions.
Solutions to Prevent Circular Contamination
Preventing circular contamination in cell culture requires a combination of strict protocols, regular monitoring, and proactive measures. Here’s how you can build a contamination-free environment:
1. Master Aseptic Techniques
The foundation of contamination prevention lies in maintaining a sterile environment.
- Biosafety Cabinets: Always perform culture handling in a properly maintained Class II biosafety cabinet to minimize airborne contaminants.
- Sterilized Equipment: Use autoclaved or pre-sterilized tools like pipettes, flasks, and culture dishes.
- Hand Hygiene: Wear gloves, sanitize hands frequently, and avoid touching non-sterile surfaces during culture handling.
2. Maintain a Clean Lab Environment
A contaminated workspace is a breeding ground for microbial growth.
- Disinfect Surfaces: Regularly clean benches, incubators, and other equipment with appropriate disinfectants like ethanol or hypochlorite solutions.
- Monitor Air Quality: Install HEPA filters in critical areas to minimize airborne contaminants.
- Dedicated Spaces: Separate cell culture areas from general-use lab spaces to reduce cross-contamination risks.
3. Ensure Media and Reagent Quality
Reagents and media are common sources of contamination.
- Use Trusted Suppliers: Source media, serum, and reagents from reliable manufacturers with rigorous quality controls.
- Inspect Before Use: Check for unusual turbidity, discoloration, or precipitates in media and reagents.
- Filter Sterilize: Pass media and solutions through 0.2 µm filters before use to remove potential contaminants.
4. Incorporate Routine Testing
Regular testing can catch contamination before it spreads.
- Mycoplasma Testing: Perform periodic PCR or ELISA tests to detect mycoplasma, one of the most elusive contaminants.
- Sterility Checks: Use sterility assays to confirm the absence of bacteria and fungi in your cultures.
- Microscopic Inspections: Routinely examine cultures under the microscope to identify early signs of microbial growth.
5. Label and Handle Cultures Carefully
Minimize handling errors and accidental cross-contamination.
- Proper Labeling: Ensure each culture vessel is clearly labeled with identifiers like cell line, passage number, and date.
- Separate Equipment: Use dedicated pipettes, media bottles, and tools for each cell line to avoid cross-contamination.
- Avoid Overcrowding: Do not overcrowd incubators or biosafety cabinets, as this increases the likelihood of contamination.
6. Use Antibiotics Judiciously
While antibiotics can suppress bacterial contamination, overuse can lead to resistant strains and mask underlying issues.
- Short-Term Use Only: Employ antibiotics as a temporary measure when contamination is suspected.
- Focus on Prevention: Aim to eliminate contamination sources rather than relying on antibiotics as a long-term solution.
Conclusion
Circular contamination in cell culture is more than just an inconvenience, it’s a significant challenge that can compromise the integrity of research and waste valuable time and resources. By understanding its causes, recognizing the warning signs, and implementing robust preventive measures, researchers can minimize the risk and maintain healthy, reliable cultures.
Whether it’s mastering aseptic techniques, routinely testing for contaminants, or taking swift action when contamination occurs, every step plays a critical role in safeguarding your work. With diligence and a proactive approach, contamination can be effectively managed, allowing you to focus on what truly matters: advancing scientific discovery and innovation.
By staying informed and vigilant, researchers can transform cell culture from a source of frustration to a foundation of success. After all, the integrity of your experiments depends on the purity of your cultures